Medical misdiagnosis is more common than many people think. While most healthcare professionals aim to provide accurate assessments, errors in diagnosing conditions can lead to prolonged illness, unnecessary treatments, or worsened health outcomes. For patients, recognizing when something feels off can be the first step in addressing a potential mistake. Learning to identify the warning signs can make a real difference in managing your care with confidence.
Trusting your instincts and pushing for answers may feel uncomfortable, but it can be vital. If symptoms persist or escalate in ways that contradict your diagnosis, your concerns deserve attention.
Persistent or Worsening Symptoms Despite Treatment
One major sign that a diagnosis may be inaccurate is when your symptoms continue or grow worse even after starting treatment. While not every treatment works immediately, most should yield some improvement within a predictable timeframe. If you’re following your care plan and noticing no positive change, or new symptoms begin to appear, it may signal that your initial diagnosis was off-target.
This is especially relevant for chronic conditions or illnesses that can mimic others in early stages. Whether it’s pain, fatigue, or neurological changes, staying alert to patterns and tracking symptoms gives your doctor more to work with during follow-up visits.
Conflicting Second Opinions
Seeking a second opinion is not just for serious illnesses. It’s a responsible step any time a diagnosis carries long-term implications or significant treatment risks. If two healthcare providers give you very different explanations for the same issue, it might be time to dig deeper.
When comparing second opinions, look beyond the diagnosis itself. Pay attention to how each provider approaches the problem, whether they rely on the same tests, and how well they explain their reasoning. Variations in interpretation can be normal, but drastically opposing views should never be ignored.
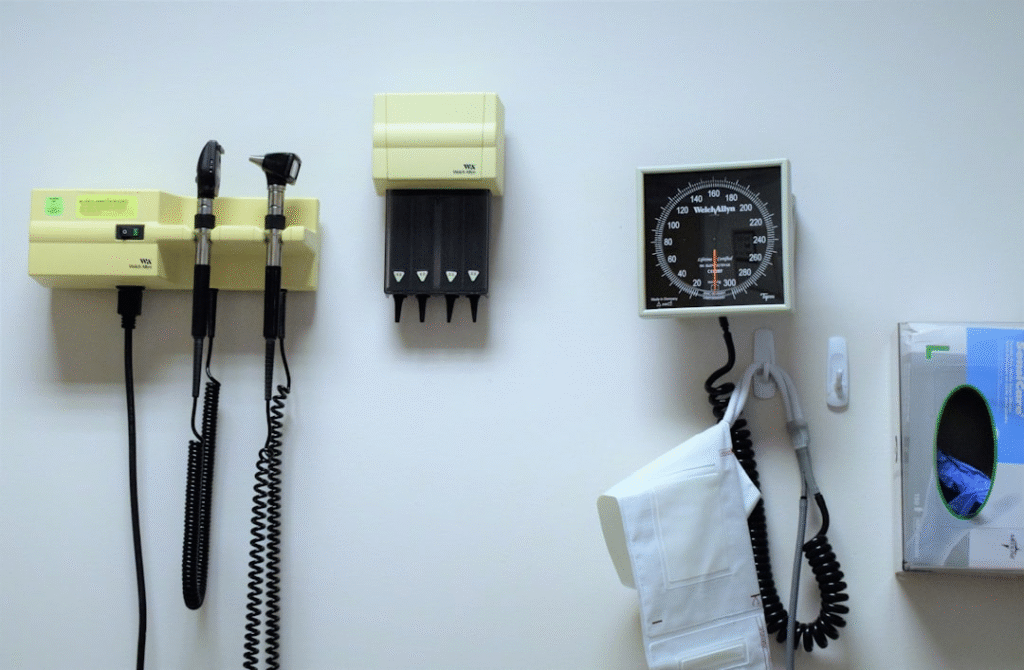
Diagnoses Without Adequate Testing
Some patients receive a diagnosis without undergoing tests that are standard for the condition. For example, being diagnosed with a gastrointestinal disorder without lab work, imaging, or endoscopy might raise questions. A careful diagnosis should include a combination of history-taking, physical examination, and diagnostic tools that rule out other possibilities.
Patients can ask their provider which conditions were considered and what steps were taken to confirm the diagnosis. If those answers are vague or incomplete, there could be room for doubt. Doctors should welcome those questions as part of collaborative care.
Symptoms That Don’t Match Common Patterns
When a condition doesn’t follow its usual course, it’s worth re-evaluating the diagnosis. Every person is different, and not all symptoms will fit a textbook definition. Still, some patterns are well established, such as the nature of a migraine or how diabetes presents in its early stages.
If your diagnosis doesn’t seem to match known characteristics of the illness, ask for clarification. Sometimes, a less common condition is missed in favor of something more familiar, which can lead to months of incorrect treatment and frustration.
Unresponsive or Dismissive Providers
Medical professionals who become defensive or dismissive when you ask questions may not be the right partner for your healthcare. A good provider will listen, explain, and involve you in decision-making. When a practitioner refuses to reconsider a diagnosis despite persistent symptoms, it can be a red flag.
Your health concerns deserve thoughtful evaluation. While doctors are under pressure in busy systems, communication should never be sacrificed. Mutual respect is key to making sure you’re on the right track with your care.
Legal Support May Be Necessary
In serious cases, especially those involving life-threatening illnesses, a misdiagnosis can cause lasting harm. If you believe your case involves medical negligence, exploring your legal options may provide clarity. Consulting a cancer misdiagnosis attorney in Michigan, for instance, can help you understand if there were failures in the diagnostic process that contributed to delayed or improper care. These professionals can evaluate records and timelines to determine if your experience meets legal criteria.
The legal aspect is not about blame, but about protection, accountability, and ensuring your needs are addressed after potential errors.
Lack of Follow-Up or Monitoring
Proper medical care involves tracking how patients respond to treatment. If your provider fails to schedule follow-ups, order repeat tests, or monitor your condition over time, a mistake could go unnoticed. A diagnosis should not be a one-time statement, but the beginning of a process that evolves with your health status.
Without follow-up, problems can compound. Symptoms might worsen, side effects might go unchecked, and incorrect assumptions remain unchallenged. This is where patients need to stay proactive and ask for updates or re-evaluation when needed.
What to Do If You Suspect a Misdiagnosis
If you think your diagnosis might be incorrect, start by documenting your symptoms, test results, and any concerns you’ve brought up during visits. Share this timeline with a new provider when seeking another opinion. Be clear, specific, and organized to give them the best chance of seeing patterns others may have missed.
Do not hesitate to ask what other conditions could explain your symptoms. Good providers appreciate thoroughness and often welcome a fresh look at the situation. Your persistence can lead to more accurate answers and better outcomes.
Being your own advocate in the healthcare system is not always easy, but it’s often necessary. Understanding the signals of a potential misdiagnosis helps you stay informed, ask the right questions, and protect your long-term health. Clear communication, proper follow-up, and timely legal or medical consultation can all play a role in getting you back on track. When diagnosis goes right, treatment has a far better chance of doing the same.