The line between “just weekends” and early dependence is blurring, and not only because of how people talk about it. New product formats, especially drinkables and so-called “functional” cocktails, are changing how intoxication shows up in everyday routines for teens and adults. What used to look like a clear choice between drinking or not drinking now shows up as a mix of alcohol, cannabis-infused beverages, nicotine, energy drinks, sedatives, and pills that move through a weekend like a relay race.
Health workers and treatment providers say the shift matters because combined use changes impairment and dependence risk, even when someone insists it’s limited to Friday and Saturday nights. The pattern often looks contained on a calendar while the effects stretch into the workweek.
A market that borrows the language of wellness
Across social media and retail shelves, products increasingly borrow cues from wellness culture: minimal branding, flavor-forward packaging, and claims that sound lifestyle-friendly. Drinkables and “functional” mixes sit alongside more familiar alcohol options, and in some circles they are treated as a lighter, more controlled form of intoxication. That framing makes early misuse easier to rationalize.
The change is not only aesthetic. When products are positioned as “better” or “cleaner,” people often downplay the role they play in mood regulation, sleep disruption, and tolerance creep. For teens, the appeal can be social, discreet, and easy to explain away. For adults, it often fits into a compressed routine that tries to balance work stress with fast relief.
Combined use changes the risk profile, even when frequency stays “weekends”
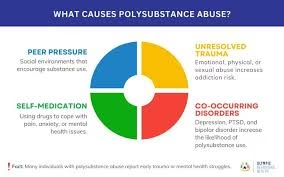
Clinicians who evaluate substance use patterns often focus less on the number of days and more on what happens within those days. Polysubstance use can mean taking multiple substances at the same time, but it also shows up as sequencing: alcohol first, then cannabis, then a sedative for sleep, then caffeine or stimulants to recover, with nicotine running through the whole cycle.
How impairment becomes harder to read
When substances interact, the subjective feeling of being “fine” can become less reliable. People often report feeling steady or in control while attention, reaction time, and judgment remain impaired. In combined-use situations, the person’s confidence can rise while performance drops, a mismatch that raises the risk of injury and driving errors.
How dependence can develop without daily use
Providers describe a common early-stage pattern: weekend-only use that gradually becomes more planned, more intense, and more medically risky. The hallmark is not necessarily weekday consumption but escalation inside the weekend window and spillover effects that affect Monday through Thursday.
Tolerance creep shows up quietly, and often looks “normal”
Tolerance creep is one of the most reported early signals in weekend-based misuse. It rarely arrives as a sudden change. It shows up as small upgrades: stronger drinks, higher-dose edibles, mixing products to “smooth it out,” or starting earlier in the day to get the same effect.
Signals that the baseline is shifting
- Needing more to get the same buzz or calm
- Using earlier in the day on weekends
- Switching to stronger forms because the old dose “does nothing”
- Adding a second substance to manage the effects of the first
- Treating intoxication less as fun and more as a way to feel steady
People often describe these shifts as practical adjustments. Clinicians tend to read them as evidence that the brain is adapting to repeated spikes in reward and sedation.
Mood rebound is emerging as a common “Monday story”
Treatment providers and mental health clinicians report that many weekend-only routines come with a predictable emotional rebound. People feel lighter or more social during the weekend, then report anxiety, irritability, low mood, and sleep disruption in the days that follow. The cycle can repeat weekly and still be described as casual.
For families, the rebound often shows up as mood volatility: a person who seems fine on Saturday night and markedly withdrawn or reactive on Monday. In households with teens, the pattern can be misread as typical adolescence or school stress until it becomes consistent and tied to weekend behavior.
Some facilities that treat overlapping substance use and mental health symptoms describe this as a “dual-track” presentation, where mood symptoms and substance patterns reinforce each other. Mental Health Treatment in California is one example of a provider that sits in that mental health treatment space.
Driving-risk myths continue, even as mixing becomes more common
Despite public awareness campaigns, familiar myths still circulate in social settings: “I drive better like this,” “I’m not that drunk,” “I waited a bit,” or “it’s just a small amount.” Clinicians note that mixed use can make self-assessment less accurate. People may feel less impaired than they are, particularly when a stimulating substance offsets sleepiness without restoring coordination and judgment.
In weekend routines that include multiple substances, the “safe enough” narrative often becomes part of the habit. Providers say the concern is not only immediate risk but also normalization, where repeated near-misses lower a person’s internal alarm system over time.
How rehab teams evaluate “it’s just weekends”
When people enter an assessment saying they only use it on weekends, providers typically track consequences and control rather than frequency alone. They focus on whether the person loses control once they start, whether recovery takes up part of the workweek, and whether the person stacks substances to manage effects.
Common markers in early polysubstance dependence
- Loss of control after the first drink or dose
- Planning the weekend around access and supply
- Hiding details from family, partners, or friends
- Repeated consequences: fights, risky decisions, injuries, missed obligations
- Using one substance to counter another (downers after stimulants, cannabis after alcohol, sedatives to sleep)
- Escalation during stress, even if weekdays remain “clean”
Rehab teams often describe weekend dependence as a pattern that can look invisible to outsiders because it sits inside socially accepted time windows. NJ Drug Addiction Rehab is one New Jersey-based example of a provider that addresses substance use patterns, including cases framed as weekend-only.
The emerging picture: a “contained” habit that spills into the week
Across age groups, clinicians and families describe a similar arc: what starts as occasional weekend intoxication becomes a structured routine with built-in escalation and recovery cycles. The system can include multiple substances, each serving a role: social confidence, mood lift, sleep, energy, appetite control, or anxiety suppression.
The headline shift is not that people use substances on weekends. It’s that the weekend has become a high-intensity container for mixed use, with products that blur intoxication and wellness language, and with aftereffects that show up in mood, sleep, and decision-making well past Sunday night.