One of the most common problems that the healthcare industry is facing lately is the exponential growth in healthcare data. Interestingly, the healthcare industry is one of those industries that has one of the highest data generation rates.
The problem that it creates is the complication it creates in integration. For instance, when you add a new system that grows geometrically and not linearly, integrating it with your system becomes much more complex.
This is where interface engineer healthcare comes into the picture. And it can simplify complex healthcare integration too quickly and effectively. Also, it helps healthcare organizations in cutting down costs on maintenance and also enables scaling ventures.
Rather than looking at interface engine healthcare as an integration, look at it as an architectural approach for your healthcare system that can transform chaos into manageable and scalable integration solutions.
On that note, let’s see how you can leverage interface engine healthcare to simplify your healthcare integration venture effectively and efficiently.
Understanding Interface Engines: The Hub-and-Spoke Solution to Healthcare Integration Chaos
The Fundamental Architecture Difference
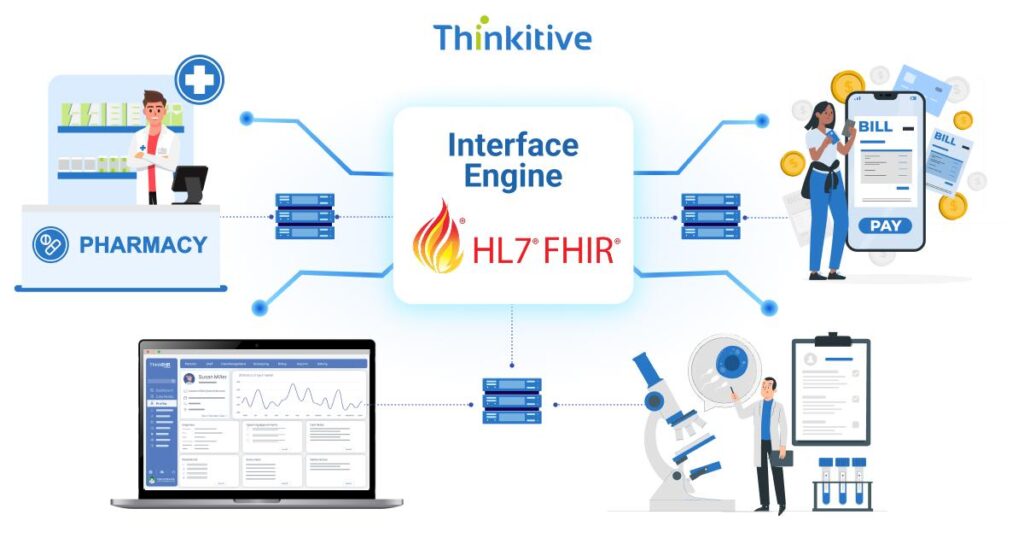
Traditionally, systems were integrated following a point-to-point integration model. Meaning that each system had to be connected with the required systems point by point. This had the potential to create an integration chaos. However, with an interface engine healthcare, all the integration points in your system are connected to a middleware, which later connects with the required system.
This hub-and-spoke model of integration not only reduces the complexity in interfaces through a centralized architecture, where standardized data transformations are used with routing capabilities to reduce development time and maintenance requirements.
Core Capabilities & Functional Components of Healthcare Interface Engine
One of the core functional components of the healthcare interface engine is its message routing and data transformation. This is used to convert data between different healthcare systems using different formats and protocols into a standardized one within a single platform. This makes error handling much easier, along with data monitoring for exchanged data.
Business Value Proposition: From Cost Center to Strategic Eabler
When you use an interface engine healthcare for EHR integration, then the project timeline can be reduced from months to weeks, as most of the components used in it are reusable and are aligned with standardized processes.
Moreover, with centralized management and standardized interface development approaches, the maintenance cost is also reduced while giving enough room for innovation and scalability.
Options You Can Choose
There are many interface engines available in the market that you can choose from, like EPIC Bridge, Cerner HealthLife, InterSystems Ensemble, etc. Though their cost can be a concern. However, you can choose open-source options as well, like Mirth Connect integration, for its healthcare-specific capabilities.
Mirth Connect Integration: Open-Source Power for Healthcare Integration
In the open-source market, Mirth Connect Integration is something that is being widely used by healthcare organizations worldwide. Here are some of the benefits that you must know about Mirth Connect Integration:
Mirth Connect’s Healthcare-Specific Features & Capabilities
The healthcare-specific feature of Mirth Connect Integration is that it uses native HL7 message processing as a standard for data exchange. Moreover, the FHIR API support has been designed specifically to address healthcare data exchange requirements.
Mirth Connect Integration can be used to optimize the user interface and development environment as it makes the connection process easier. Moreover, with extensive healthcare protocol support, including DICOM, NCPCP, and proprietary EHR interfaces, Mirth Connect offers the perfect solution for EHR integration with open source.
Cost Advantage & Total Cost of Ownership Benefits
The cost advantage you get with Mirth Connect Integration is that you eliminate the vendor fees completely. So even if you’re using it at enterprise-grade, you can get advanced EHR integration capabilities for a much lower cost.
And since it is a community-driven development, you can be assured of continuous innovation and up-to-date technological advancements with healthcare industry-specific enhancements.
Implementation Flexibility & Customization Capabilities
Mirth Connect Integration is a JavaScript-based healthcare interface engine. Due to JavaScript’s robust logic development capabilities, your system can easily process complex healthcare data processing.
Moreover, with a plugin architecture that supports custom connectors, you can easily streamline and satisfy your specialized healthcare integration needs.
Technical Architecture & Implementation Benefits
Now, let’s have a look at the technical architecture required for interface engine healthcare and how it can benefit your healthcare integration.
Centralized Data Transformation & Standardization Capabilities
Interface engine healthcare uses a single point of control for healthcare systems, such as data mapping, validation, and transformation. This alone can reduce inconsistencies and errors by a significant margin. Furthermore, with the use of reusable transformation components accelerating the development of new healthcare integrations, the overall maintenance overhead is reduced.
All these activities use data quality through centralized validation and cleansing processes that are applied to all healthcare data exchanges.
Protocol Agnostic Connectivity Supporting Diverse Healthcare Systems
The best part about using interface engines is that they provide native support for healthcare protocols like HL7 and FHIR. Along with that, it also supports standard IT protocols like HTTP, FTP, and databases in a unified platform. Furthermore, with legacy system integration capabilities, you can easily integrate with older systems without having the need to replace the system integration.
Scalability, Performance, Security & Compliance Features
Interface engines are often associated with supporting high-volume healthcare data processing and transaction loads, which is because of its horizontal scaling capabilities. Along with that, with features like load balancing and failover capabilities, continuous integration can be achieved, which also enables performance monitoring and providers optimization tools to enhance the system performance.
Along with that, with healthcare-specific security controls supporting HIPAA Compliance, PHI protection requirements are easily satisfied. This also helps in audit logging by enabling tracking and providing comprehensive visibility into healthcare data access and modifications.
Moreover, with the implications of encryptions with secure communication protocols, you can ensure that your healthcare data is protected during both transmission and processing.
Simplifying Complex Integration Scenarios Through Interface Engine Architecture
Let’s dive deep into the interface engine architecture and how it simplifies complex integration scenarios for your healthcare software systems:
Multi-EHR Environment Management & Data Harmonization
If you are looking for a multi-EHR integration solution, then you need an interface engine healthcare platform to manage multiple EHR interactions through centralized middleware. Moreover, with data standardization and normalization capabilities, you can ensure consistent patient information storage across diverse healthcare systems.
Furthermore, with master patient index management and patient matching capabilities, addressing issues related to patient identity can be resolved across multiple systems.
Department-Specific System Integration & Workflow Optimization
As a healthcare practice, you naturally have to connect with multiple healthcare systems to exchange data and information on a regular basis. Some of such systems include laboratory, radiology, pharmacy, and specialty systems. This can be achieved seamlessly with a centralized interface engine architecture.
In short, you will have one specific point for all your systems to integrate. Moreover, by coupling this data routing and notifications, your workflow can be optimized to a great extent, and a reduction in manual interventions can be seen. This boosts care coordination and enhances real-time data sharing with clinical alert distribution across departments.
Cloud Migration & Hybrid Architecture Support
Many assume that the healthcare interface engine only supports cloud-based architecture or on-premise legacy systems. However, it’s quite the contrary. You see, in many system interface engines, healthcare platforms act as a bridge between on-premise legacy systems and cloud-based applications. API gateway functionality enables this capability while facilitating secure and controlled access to healthcare data for both cloud and mobile applications.
Implementation Strategy & Best Practices for Healthcare Interface Engines
Healthcare interface engine implementation is a lengthy and a little more complex process than it seems on the surface. So, here are some of the strategies and best practices that you must consider while implementing an interface engine healthcare platform:
- Planning & Assessment Methodologies: Assess your current system and identify existing flaws in interfaces, data flows, and pain points that are there in your system. Then, fill the gaps by redesigning the architecture and plan an optimal interface engine with a solid integration strategy.
- Phased Implementation Approaches: Divide the implementation process into smaller milestones and implement them accordingly so that you can strategically move your existing interfaces to a centralized platform while maintaining operational continuity.
- Team Structure & Skill Development: Then you also need to train your team on effective use of the healthcare interface engine platform. Along with that, there would be role-specific roles and responsibilities that you also need to assign and train accordingly.
- Governance & Maintenance Framework: This needs to be done to ensure that your interface engine healthcare system is always in compliance with the regulatory standards and its performance is always top-notch.
Conclusion
Interface engine healthcare platforms can be your key to establishing integration with multiple healthcare systems easily and without creating a fuss of the network. On that note, establishing connectivity reduces your cost and accelerates innovations that can strategically place your system at an advantage in the healthcare delivery landscape.
So, what are you waiting for? Let’s get started today, click here to start with your current system assessment.
FAQs
- What are the key differences between interface engines and point-to-point integration approaches in healthcare?
Point-to-point integration involves direct, custom connections between two systems, becoming complex and difficult to manage as more systems are added. Interface engines, conversely, act as a central hub, translating and routing data between multiple systems. This offers better scalability, centralized management, and reduced long-term costs.
- How does Mirth Connect integration compare to commercial interface engine solutions for healthcare organizations?
Mirth Connect, traditionally open-source, offers cost-effectiveness and strong HL7/FHIR support. Commercial solutions often provide more robust features, dedicated vendor support, and easier scalability for complex enterprise needs, albeit at a higher cost. Mirth Connect’s recent shift to a commercial licensing model for newer versions blurs this distinction.
- What are the typical implementation timelines and resource requirements for healthcare interface engine projects?
Typical healthcare interface engine projects range from 3-6 months for initial connections, extending for complex enterprise-wide implementations. Key resources include a dedicated project manager, interface analysts/developers with HL7/FHIR expertise, IT infrastructure support, and active involvement from clinical and operational stakeholders for requirements gathering and testing.
- How do interface engines support HIPAA compliance and healthcare data security requirements?
Interface engines support HIPAA compliance by enabling secure data exchange through encryption, access controls, and audit logging. They transform and route protected health information (PHI) between disparate systems while adhering to healthcare standards like HL7 and FHIR, minimizing manual errors and unauthorized access, thereby enhancing data security.
- What are the ongoing maintenance and support requirements for healthcare interface engine implementations?
Ongoing maintenance for healthcare interface engines includes continuous monitoring, scheduled updates/testing, backup/disaster recovery, and performance optimization. Support involves documentation, training, and 24/7 assistance to ensure smooth, secure, and compliant data exchange between disparate healthcare systems.
- How can healthcare organizations measure ROI from interface engine investments?
Healthcare organizations measure interface engine ROI by tracking quantifiable benefits like reduced manual data entry errors, decreased administrative costs, improved efficiency in data exchange (e.g., faster billing cycles, reduced denial rates), and enhanced clinical workflows. Comparing these savings/gains against implementation and ongoing maintenance costs reveals the ROI.
- What technical skills and team structure are needed for successful interface engine healthcare implementations?
Successful healthcare interface engine implementations require technical skills in HL7/FHIR standards, data mapping/transformation, and the specific interface engine (e.g., Mirth, Rhapsody). The ideal team includes a project manager, interface analysts/developers, QA specialists, and clinical subject matter experts to ensure alignment with workflows and patient care.
- How do interface engines support cloud migration and hybrid healthcare IT architectures?
Interface engines act as central hubs, translating and routing data between disparate systems (on-premise and cloud-based). They standardize data formats (e.g., HL7, FHIR), enabling seamless exchange for cloud migration and hybrid architectures. This ensures interoperability, security, and scalability across diverse healthcare IT environments
- What are the scalability considerations for interface engines in large healthcare organizations?
Scalability for healthcare interface engines involves handling high message volumes, supporting diverse data formats (HL7, FHIR), ensuring low latency, and accommodating new integrations and systems as the organization grows. This requires robust architecture, potentially cloud-based solutions, and efficient error handling.
- How do interface engines handle healthcare-specific protocols like HL7 and FHIR?
Interface engines act as translators, converting healthcare data between disparate systems using various protocols. For HL7, they parse and transform its segmented, delimited messages. For FHIR, they leverage its modern, resource-based RESTful APIs and handle data in formats like JSON or XML. They map data elements, ensuring seamless and standardized exchange.
- What are the key selection criteria for choosing between different interface engine healthcare solutions?
Key selection criteria for healthcare interface engines include: interoperability (HL7, FHIR support), scalability, data security/compliance (HIPAA), ease of use (low-code/no-code capabilities), total cost of ownership, vendor support, and reliability/uptime.
- How do interface engines support healthcare regulatory reporting and compliance requirements?
Interface engines centralize data exchange between disparate healthcare systems, translating formats (e.g., HL7, FHIR). This streamlines data flow for regulatory reports, ensuring accuracy, timeliness, and completeness. They support compliance by enabling consistent, secure data sharing, automating reporting processes, and maintaining audit trails, reducing manual effort and errors.